


In Vitro fertilisation, also known as IVF, is a fertility treatment where in fertilisation takes place in the lab instead of the female body.
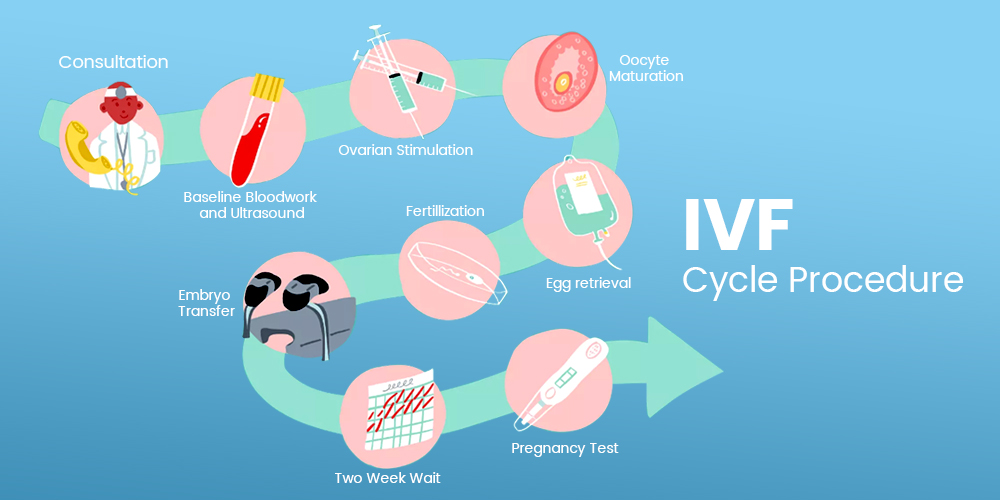
The basic steps involved in IVF technology is taking many eggs from female retrieved through transvaginal ultrasound-guided needle and placing in a petri-dish with cleanly washed sperm cells retrieved via masturbation or else sperm donor. The retrieved eggs will become fertilized by the sperm cells and become embryos. One of the healthy embryo is then transferred to the same female uterus. After process completion, bed rest is advised for at least 24 hrs.
An estimated 6.5 million IVF conceived babies have been born in the world since IVF conception in 1980s. Also famously known as test tube babies, produced by IVF are as healthy and normal as naturally conceived children.
Success rate of IVF, according to a study of approximately 156,000 women, the average live-birth rate for the first cycle was 29.5 percent, which is a comparable success ratio as that to couples with the natural cycle of fertility. Researchers in the UK have developed a prediction model to estimate the success rate of a live birth over multiple cycles of IVF. This prediction model can be personalized based on a number of variables (reproductive history, maternal age, the cause of infertility, and lifestyle factors) as well as their response to treatment for a realistic understanding of the long-term probability of success of IVF.
IVF is the preferred choice of treatment in the following health conditions:
Further, obesity can also complicate IVF, making it harder for overweight women to have successful IVF with their own eggs. Obesity is associated with increased dose and duration of gonadotropin stimulation, lower peak E2 levels, and increased oocyte retrieval time.
A large study published in 2013 reviewed over 9,500 egg donation IVF treatments. The egg donors were all of normal weight, and the recipients were divided into four groups: underweight, normal, overweight and obese. The rates of embryo implantation reduced to 23%, pregnancy rate decreased by 19% and live birth percentage reduced by 27% as body mass index (BMI), increased to obese.
A recent study indicated that obese women may need different doses and dosing regimen and fertility drugs than normal-weight women in order to ensure that their eggs ripen at the right time and can be extracted for IVF.
Therefore, it is recommended that patients with a high BMI reduce their weight before IVF treatment. Bariatric surgical procedures can be a durable option for weight reduction. This study highlights 5 patients who underwent Roux-en-Y gastric bypass bariatric surgery followed by in vitro fertilisation (IVF). Overall, these patients tolerated IVF well, and four of the five went on to have term deliveries. Rapid weight loss and increased risk of nutritional deficiencies in the first year after bariatric surgery have led to recommendations that gastric bypass surgery patients should wait at least a year before attempting pregnancy. IVF after bariatric surgery can be safe and successful.
Related Articles
PCO combined with obesity – A major cause for infertility Bariatric surgery leads to higher probabilities for conception
Great, I really like it! Youre awesome
Thanks for your feedback.
Thanks for sharing this wonderful information with us.
Thanks For Sharing Your Feedback.
Hi,
Very nice informative article. Thanks a lot for sharing this good information. The IVF advanced is one of the most excellent centers in Asia Pacific, with Techniques, genuine Treatment, Research & Training. The IVF advanced is the leading Test Tube Centre in the country with modern world-class scientific technologies.
Thanks For Sharing Your Feedback.